My mom passed away earlier this month. I realize now that her legacy isn’t just in what she did during her life, it’s in who I am in mine.
As with so much of our Alzheimer’s journey, it was a slow moving end. She was just subtly different one day to the next and I found myself in a strange(r) waiting period for several months. I spent a lot of time sitting with her – sometimes she was awake, but often she slept – and thinking. After all these years, my brain can’t understand that she is gone. I knew she was mortal – though she did have a knack for making me question that – but it’s still a complete mental doozy. Grief in the traditional form of reckoning with her absence from this Earth altogether sits in my peripheral vision. It’s there, but somehow I am not ready for it yet.
There are so many threads to pull on from these last several months that merit further reflection, but the most revelatory at this stage for me is the idea of my mom’s legacy. I have always known how much I loved my mom and how deeply she cared about me and my brothers. Through the lens of her life in review, which somehow only became more accessible when the end was approaching, I see more clearly what she passed on to me. There are obvious things, like my eye color and my curly hair. And then there are the more subtle, nurture things. As I worked to capture who my mom was in her obituary, all the ways she served her community became abundantly clear. I was telling someone just yesterday that one of the first things I did when I got to college was to join the student volunteer center. It struck me then how my mom quietly did her thing and influenced the person I became without me even really noticing it. In other ways she was more overt. I have thought a lot over the years about how freaked out she was when I took a semester off from college. She worried that I wouldn’t go back. All this time I’ve maintained the narrative, “Didn’t she know me at all? I was always going to go back.”

But, now, I see it more clearly. It didn’t have to do, exactly, with knowing me. It was about what she wanted for me. She did everything she could for our entire lives to make sure my brothers and I had a smoother path and better opportunities than she did. She graduated from college when she was 49 years old. I was 16. It could not have been easy with 3 kids, our endless sports schedules, and her school work – and yet she still managed to get us where we needed to be and to put dinner on the table. She wanted me to finish college while I was still young and unencumbered, to just have that college degree in my back pocket.
It makes me think about the parents of the Girl Pioneers at MAIA that I work with in Guatemala. By choosing to educate their daughters, they chart a different path for their families with the hope of improving the future for the next generation. This path is unfamiliar to them and requires real courage, commitment and selflessness. But they want better for their children so they take a chance on this opportunity.
Several years ago MAIA ran a fundraising campaign called Nim Mama, which means “Great Mother” in the Maya Kaqchikel language of this region of Guatemala. The campaign focused on honoring mothers and their collective strength, beauty, and transformative power. The images of the pioneering, brave girls of MAIA with their mothers at their side brought me to tears. They reflected back to me my own mom’s strength and guiding light and reminded me how important my education was to her.
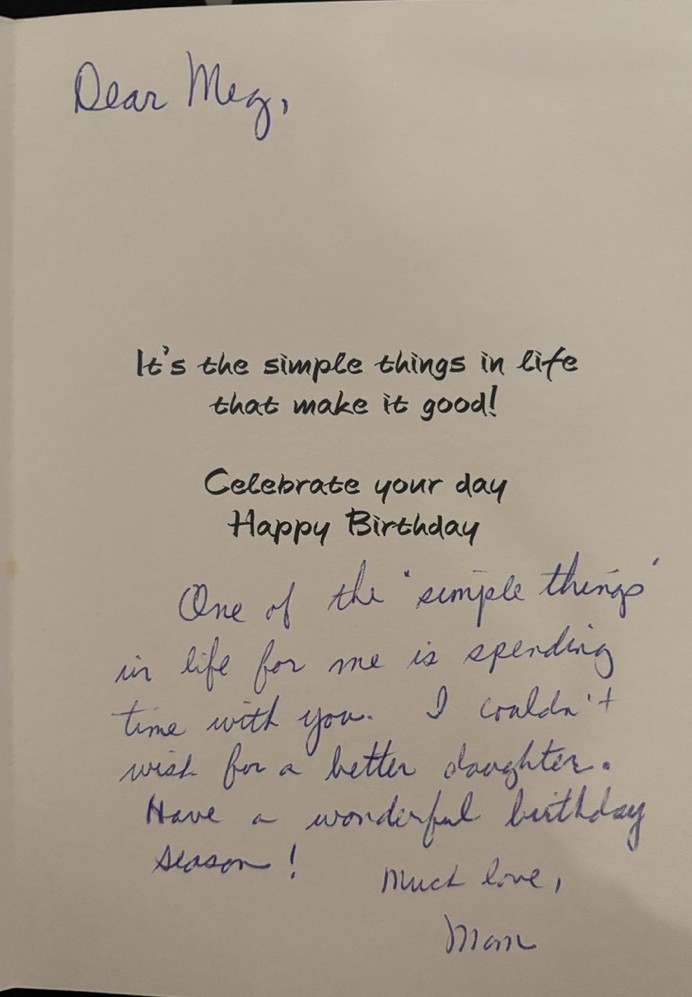
As I go through old photos of me and my mom I think about the legacy of what she gave to me. She stood alongside me, literally or figuratively, my whole life in the same way that the mothers of MAIA stand alongside their pioneering daughters. I realize now that my mom will live on through me – in who I am, in how I tell her story, and by paying it forward like she did so that the next generation has more opportunities and a smoother path still than I did.


I am the same age now that my mom was when she graduated from college. I have two great kids and a loving husband. That college degree that I earned at 22 has opened doors for me. As her primary caregiver for the last decade, our roles reversed for a while as I became more and more responsible for her well-being. I accompanied her to her last day on this Earth to the best of my ability. And I know she is proud of all of these things. It helps me to imagine that she can see it all now and can feel really good about how well she guided my way.
I turn 50 next week. As my way of celebrating my 50 years on this Earth as well as the nearly 50 years I got to spend with my mom, I’m raising funds for MAIA. Paying it forward for the next generation is the best gift I can imagine receiving. Please consider joining me. https://donorbox.org/meg-s-50th-birthday-fundraiser-for-maia-guatemala